Thriving in Space: Ensuring the Future of Biological and Physical Sciences Research: A Decadal Survey for 2023-2032. National Academies of Sciences, Engineering, and Medicine, Sciences (2023).
Afshinnekoo, E. et al. Fundamental biological features of spaceflight: advancing the field to enable deep-space exploration. Cell 184, 6002 (2021).
Patel, Z. S. et al. Red risks for a journey to the red planet: the highest priority human health risks for a mission to Mars. NPJ Microgravity 6, 33 (2020).
Space Radiation and Astronaut Health: Managing and Communicating Cancer Risks. The National Academies Press (2021).
Zeitlin, C. & La Tessa, C. The role of nuclear fragmentation in particle therapy and space radiation protection. Front. Oncol. 6, 65 (2016).
Space Radiation: An Important Concern for Human Spaceflight. Space Radiation Analysis Group, Johnson Space Center. https://srag.jsc.nasa.gov/spaceradiation/why/why.cfm
Cucinotta, F. A. Space radiation risks for astronauts on multiple International Space Station missions. PLoS ONE 9, e96099 (2014).
Locke, P. A. & Weil, M. M. Personalized cancer risk assessments for space radiation exposures. Front. Oncol. 6, 38 (2016).
NASA Space Flight Human-System Standard Volume 1 Crew Health. NASA-STD-3001, Vol 1 Rev B (NASA, 2022).
Beheshti, A. et al. Genomic changes driven by radiation-induced DNA damage and microgravity in human cells. Int. J. Mol. Sci. (2021).
Meier, M. M. et al. Impact of the South Atlantic Anomaly on radiation exposure at flight altitudes during solar minimum. Sci. Rep. 13, 9348 (2023).
Federal Aviation Administration. CARI-7 and CARI-7A (2021) https://www.faa.gov/data_research/research/med_humanfacs/aeromedical/radiobiology/cari7
Scheibler, C. et al. Cancer risks from cosmic radiation exposure in flight: a review. Front. Public Health 10, 947068 (2022).
The RadLab Portal and the RadLab Data API. NASA. https://visualization.osdr.nasa.gov/radlab/gui/data-overview/ (2024).
Bottollier-Depois, J. F. et al. Assessing exposure to cosmic radiation during long-haul flights. Radiat. Res. 153, 526–532 (2000).
Papadopoulos, A. et al. Space radiation quality factor for Galactic Cosmic Rays and typical space mission scenarios using a microdosimetric approach. Radiat. Environ. Biophys. 62, 221–234 (2023).
Trovati, S. et al. Human exposure to space radiation: role of primary and secondary particles. Radiat. Prot. Dosimetry 122, 362–366 (2006).
Neumaier, T. et al. Evidence for formation of DNA repair centers and dose-response nonlinearity in human cells. Proc. Natl. Acad. Sci. USA 109, 443–448 (2012).
Jones, J., Karouia F., Cristea, O., Casey, R. & Popov, D. Ionizing Radiation as a Carcinogen, In Comprehensive Toxicology, Vol. 3rd, (ed McQueen, C.) 183–225 (Elsevier, 2018).
Vadhavkar, N. et al. Combinatorial DNA damage pairing model based on X-ray-induced foci predicts the dose and LET dependence of cell death in human breast cells. Radiat. Res. 182, 273–281 (2014).
Clowdsley, M. S. et al. Neutron environments on the Martian surface. Phys. Med. 17, 94–96 (2001).
Hassler, D. M. et al. Mars’ surface radiation environment measured with the Mars Science Laboratory’s Curiosity rover. Science 343, 1244797 (2014).
Zeitlin, C. et al. Measurements of energetic particle radiation in transit to Mars on the Mars Science Laboratory. Science 340, 1080–1084 (2013).
Zeitlin, C. et al. Measurements of radiation quality factor on Mars with the Mars Science Laboratory Radiation Assessment Detector. Life Sci. Space Res. 22, 89–97 (2019).
Nelson, G. A. Space radiation and human exposures, a primer. Radiat. Res. 185, 349–358 (2016).
Datta, K., Suman, S., Kallakury, B. V. & Fornace, A. J. Exposure to heavy ion radiation induces persistent oxidative stress in mouse intestine. PLoS ONE 7, e42224 (2012).
Kim, J. & Seli, E. Mitochondria as a biomarker for IVF outcome. Reproduction 157, R235–R242 (2019).
May-Panloup, P. et al. Ovarian ageing: the role of mitochondria in oocytes and follicles. Hum. Reprod. Update 22, 725–743 (2016).
Guzeloglu-Kayisli, O. et al. Long-acting progestin-only contraceptives enhance human endometrial stromal cell expressed neuronal pentraxin-1 and reactive oxygen species to promote endothelial cell apoptosis. J. Clin. Endocrinol. Metab. 99, E1957–E1966 (2014).
Drago-Ferrante, R. et al. Extraterrestrial gynecology: could spaceflight increase the risk of developing cancer in female astronauts? An updated review. Int. J. Mol. Sci. (2022).
Shin, E. et al. Organ-specific effects of low dose radiation exposure: a comprehensive review. Front. Genet. 11, 566244 (2020).
Adriaens, I., Smitz, J. & Jacquet, P. The current knowledge on radiosensitivity of ovarian follicle development stages. Hum. Reprod. Update 15, 359–377 (2009).
Mishra, B., Ortiz, L. & Luderer, U. Charged iron particles, components of space radiation, destroy ovarian follicles. Hum. Reprod. 31, 1816–1826 (2016).
Mishra, B., Ripperdan, R., Ortiz, L. & Luderer, U. Very low doses of heavy oxygen ion radiation induce premature ovarian failure. Reproduction 154, 123–133 (2017).
Mishra, B., Lawson, G. W., Ripperdan, R., Ortiz, L. & Luderer, U. Charged-iron-particles found in galactic cosmic rays are potent inducers of epithelial ovarian tumors. Radiat. Res. 190, 142–150 (2018).
Wallace, W. H., Thomson, A. B., Saran, F. & Kelsey, T. W. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int. J. Radiat. Oncol. Biol. Phys. 62, 738–744 (2005).
Wallace, W. H., Thomson, A. B. & Kelsey, T. W. The radiosensitivity of the human oocyte. Hum. Reprod. 18, 117–121 (2003).
Ogilvy-Stuart, A. L. & Shalet, S. M. Effect of radiation on the human reproductive system. Environ. Health Perspect. 101, 109–116 (1993).
Jensen, P. T. & Froeding, L. P. Pelvic radiotherapy and sexual function in women. Transl. Androl. Urol. 4, 186–205 (2015).
Milgrom, S. A. et al. Acute effects of pelvic irradiation on the adult uterus revealed by dynamic contrast-enhanced MRI. Br. J. Radiol. 86, 20130334 (2013).
Larsen, E. C. et al. Radiotherapy at a young age reduces uterine volume of childhood cancer survivors. Acta Obstet. Gynecol. Scand. 83, 96–102 (2004).
Van de Loo, L. E. X. M. et al. Uterine function, pregnancy complications, and pregnancy outcomes among female childhood cancer survivors. Fertil. Steril. 111, 372–380 (2019).
Papatheodorou, S. et al. Residential radon exposure and hypertensive disorders of pregnancy in Massachusetts, USA: a cohort study. Environ. Int. 146, 106285 (2021).
VanKoevering, K. K. et al. Pituitary dysfunction after radiation for anterior skull base malignancies: incidence and screening. J. Neurol. Surg. B Skull Base 81, 75–81 (2020).
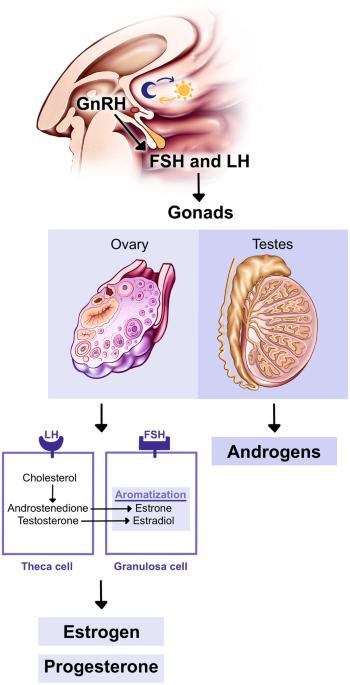
Darzy, K. H. & Shalet, S. M. Hypopituitarism following radiotherapy. Pituitary 12, 40–50 (2009).
Roth, C., Lakomek, M., Schmidberger, H. & Jarry, H. Cranial irradiation induces premature activation of the gonadotropin-releasing-hormone. Klin. Padiatr. 213, 239–243 (2001).
Gallagher, M., Torok, A., Klaas, J. & Ferrè, E. R. Gravity prior in human behaviour: a perceptual or semantic phenomenon? Exp. Brain Res. 238, 1957–1962 (2020).
Karouia, F., Peyvan, K. & Pohorille, A. Toward biotechnology in space: High-throughput instruments for in situ biological research beyond Earth. Biotechnol. Adv. 35, 905–932 (2017).
Williams DR. A crewed mission to Mars. NASA Goddard Space Flight Center. https://nssdc.gsfc.nasa.gov/planetary/mars/marsprof.html (2015).
Lin, X. et al. The impact of spaceflight and simulated microgravity on cell adhesion. Int. J. Mol. Sci.(2020).
Najrana, T. & Sanchez-Esteban, J. Mechanotransduction as an adaptation to gravity. Front. Pediatr. 4, 140 (2016).
Tuday, E. C., Nyhan, D., Shoukas, A. A. & Berkowitz, D. E. Simulated microgravity-induced aortic remodeling. J. Appl. Physiol. 106, 2002–2008 (2009).
Arbeille, P., Provost, R. & Zuj, K. Carotid and femoral artery intima-media thickness during 6 months of spaceflight. Aerosp. Med. Hum. Perform. 87, 449–453 (2016).
Page, S. & Rollins M. Physiology and Pharmacology of Obstetrics Anesthesia. In Pharmacology and Physiology for Anesthesia Foundations and Clinical Application (eds Hemmings, H. C. & Egan, T. D.) 2nd Ed., pp 732–751 (Elsevier, 2019).
Jennings, R. T. & Baker, E. S. Gynecological and reproductive issues for women in space: a review. Obstet. Gynecol. Surv. 55, 109–116 (2000).
Gillman, M. W. Developmental origins of health and disease. New Engl. J. Med. 353, 1848–1850 (2005).
Moustafa, A. Hindlimb unloading-induced reproductive suppression via downregulation of hypothalamic Kiss-1 expression in adult male rats. Reprod. Biol. Endocrinol. 19, 37 (2021).
Kramer, L. A. et al. Intracranial effects of microgravity: a prospective longitudinal MRI study. Radiology 295, 640–648 (2020).
Lauria, L., Ballard, T. J., Caldora, M., Mazzanti, C. & Verdecchia, A. Reproductive disorders and pregnancy outcomes among female flight attendants. Aviat. Space Environ. Med. 77, 533–539 (2006).
Radowicka, M., Pietrzak, B. & Wielgoś, M. Assessment of the occurrence of menstrual disorders in female flight attendants—preliminary report and literature review. Neuro Endocrinol. Lett. 34, 809–813 (2013).
Sandler, H. & Winters, D. Physiological Responses of Women to Simulated Weightlessness. A Review of the Significant Findings of the First Female Bed Rest Study (NASA SP-340, 1978).
Hong, X. et al. Effects of spaceflight aboard the International Space Station on mouse estrous cycle and ovarian gene expression. NPJ Microgravity 7, 11 (2021).
Ronca, A. E. et al. Effects of sex and gender on adaptations to space: reproductive health. J. Womens Health 23, 967–974 (2014).
Holets, L. M., Gupta, V., Roby, K. F. & Tash, J. S. Spaceflight Inhibits Ovarian Follicle Development, Induces Down Regulation of Estrogen Receptor Alpha, and Alters Metabolic Pathways and Gene Expression in Mouse Uterus. Biol. Reprod. 87, 18 (2012).
Rosa-Caldwell, M. E. et al. The oestrous cycle and skeletal muscle atrophy: investigations in rodent models of muscle loss. Exp. Physiol. 106, 2472–2488 (2021).
Megory, E., Konikoff, F., Ishay, J. S. & Lelyveld, J. Hypergravity: its effect on the estrous cycle and hormonal levels in female rats. Life Sci. Space Res. 17, 213–218 (1979).
Zwart, S. R., Auñón-Chancellor, S. M., Heer, M., Melin, M. M. & Smith, S. M. Albumin, oral contraceptives, and venous thromboembolism risk in astronauts. J. Appl. Physiol. 132, 1232–1239 (2022).
Eyal, S. & Derendorf, H. Medications in space: in search of a pharmacologist’s guide to the galaxy. Pharm. Res. 36, 148 (2019).
Davis, S. R. et al. Menopause. Nat. Rev. Dis. Primers 1, 15004 (2015).
Stavnichuk, M., Mikolajewicz, N., Corlett, T., Morris, M. & Komarova, S. V. A systematic review and meta-analysis of bone loss in space travelers. NPJ Microgravity 6, 13 (2020).
Lloyd, S. A. et al. Effect of proton irradiation followed by hindlimb unloading on bone in mature mice: a model of long-duration spaceflight. Bone 51, 756–764 (2012).
Aydogan Mathyk, B., Alvarado, F., Young, S., Beheshti, A. & Quaas, A. Effects of Spaceflight on Estrogen Receptor Expression and Signaling. Scientific Papers Presented at the 70th Annual Meeting of the Pacific Coast Reproductive Society March 23-27, 2022. Fertility and Sterility. Vol 118, e21 (2022).
Cirelli, E. et al. Effect of microgravity on aromatase expression in sertoli cells. Sci. Rep. 7, 3469 (2017).
Aydogan Mathyk, B., Alvarado, F., Young, S., Quaas, A. & Beheshti, A. Expression of insulin resistance related genes during spaceflight. Fertility Sterility 116, E107 (2021).
Mathyk, B. et al. Spaceflight induces changes in gene expression profiles linked to insulin and estrogen. Commun. Biol. https://doi.org/10.1038/s42003-023-05213-2 (2024).
Baker, F. C. & Driver, H. S. Circadian rhythms, sleep, and the menstrual cycle. Sleep Med. 8, 613–622 (2007).
Kloss, J. D., Perlis, M. L., Zamzow, J. A., Culnan, E. J. & Gracia, C. R. Sleep, sleep disturbance, and fertility in women. Sleep Med. Rev. 22, 78–87 (2015).
Caetano, G. et al. Impact of sleep on female and male reproductive functions: a systematic review. Fertil. Steril. 115, 715–731 (2021).
Wiegand, S. J. & Terasawa, E. Discrete lesions reveal functional heterogeneity of suprachiasmatic structures in regulation of gonadotropin secretion in the female rat. Neuroendocrinology 34, 395–404 (1982).
Casey, T. et al. Hypergravity disruption of homeorhetic adaptations to lactation in rat dams include changes in circadian clocks. Biol. Open 1, 570–581 (2012).
Ranieri, D., Cucina, A., Bizzarri, M., Alimandi, M. & Torrisi, M. R. Microgravity influences circadian clock oscillation in human keratinocytes. FEBS Open Bio 5, 717–723 (2015).
Fujita, S. I., Rutter, L., Ong, Q. & Muratani, M. Integrated RNA-seq analysis indicates asynchrony in clock genes between tissues under spaceflight. Life (2020).
Wang, L. et al. NR1D1 targeting CYP19A1 inhibits estrogen synthesis in ovarian granulosa cells. Theriogenology 180, 17–29 (2022).
Pavlovic, M. V., Marinkovic, D. Z., Andric, S. A. & Kostic, T. S. The cost of the circadian desynchrony on the Leydig cell function. Sci. Rep. 12, 15520 (2022).
Touzet, S., Rabilloud, M., Boehringer, H., Barranco, E. & Ecochard, R. Relationship between sleep and secretion of gonadotropin and ovarian hormones in women with normal cycles. Fertil. Steril. 77, 738–744 (2002).
Vgontzas, A. N. et al. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: clinical implications. J. Clin. Endocrinol. Metab. 86, 3787–3794 (2001).
Breen, K. M. & Mellon, P. L. Influence of stress-induced intermediates on gonadotropin gene expression in gonadotrope cells. Mol. Cell Endocrinol. 385, 71–77 (2014).
Jiang, Z. et al. Aging attenuates the ovarian circadian rhythm. J. Assist. Reprod. Genet. 38, 33–40 (2021).
Werdermann, M. et al. Insulin and obesity transform hypothalamic-pituitary-adrenal axis stemness and function in a hyperactive state. Mol. Metab. 43, 101112 (2021).
Oosterman, J. E., Wopereis, S. & Kalsbeek, A. The circadian clock, shift work, and tissue-specific insulin resistance. Endocrinology (2020).
Hughson, R. L. et al. Increased postflight carotid artery stiffness and inflight insulin resistance resulting from 6-mo spaceflight in male and female astronauts. Am. J. Physiol. Heart Circ. Physiol. 310, H628–638, (2016).
St-Onge, M. P. et al. The interrelationship between sleep, diet, and glucose metabolism. Sleep Med. Rev 69, 101788 (2023).
Dupont, J. & Scaramuzzi, R. J. Insulin signalling and glucose transport in the ovary and ovarian function during the ovarian cycle. Biochem. J. 473, 1483–1501 (2016).
Silvestris, E., de Pergola, G., Rosania, R. & Loverro, G. Obesity as disruptor of the female fertility. Reprod. Biol. Endocrinol. 16, 22 (2018).
Caughey A. B. ACOG Practice Bulletin No. 180: Gestational Diabetes Mellitus. American College of Obstetricians and Gynecologists. Obstet. Gynecol. 130, e17–e37. https://journals.lww.com/greenjournal/fulltext/2017/07000/practice_bulletin_no__180__gestational_diabetes.51.aspx (2017).
Fekry, B. & Eckel-Mahan, K. The circadian clock and cancer: links between circadian disruption and disease Pathology. J. Biochem. 171, 477–486 (2022).
Orisaka, M. et al. The role of pituitary gonadotropins and intraovarian regulators in follicle development: a mini-review. Reprod. Med. Biol. 20, 169–175 (2021).
Cheng, K. et al. Simulated microgravity reduces quality of ovarian follicles and oocytes by disrupting communications of follicle cells. NPJ Microgravity 9, 7 (2023).
Dai, T. X. et al. Simulated microgravity induces the proliferative inhibition and morphological changes in porcine granulosa cells. Curr. Issues Mol. Biol. 43, 2210–2219 (2021).
Gorbacheva, E. Y. et al. The state of the organs of the female reproductive system after a 5-day “dry” immersion. Int. J. Mol. Sci. (2023).
Zhang, S. et al. Simulated microgravity using a rotary culture system compromises the in vitro development of mouse preantral follicles. PLoS ONE 11, e0151062 (2016).
Wu, C. et al. Simulated microgravity compromises mouse oocyte maturation by disrupting meiotic spindle organization and inducing cytoplasmic blebbing. PLoS ONE 6, e22214 (2011).
Miglietta, S. et al. Effects of simulated microgravity in vitro on human metaphase II oocytes: an electron microscopy-based study. Cells (2023).
Lemseffer, Y., Terret, M. E., Campillo, C. & Labrune, E. Methods for assessing oocyte quality: a review of literature. Biomedicines (2022).
Ferreira, A. F., Soares, M., Almeida-Santos, T., Ramalho-Santos, J. & Sousa, A. P. Aging and oocyte competence: a molecular cell perspective. WIREs Mech. Dis. 15, e1613 (2023).
Luxton, J. J. et al. Telomere length dynamics and DNA damage responses associated with long-duration spaceflight. Cell Rep. 33, 108457 (2020).
Capri, M. et al. Long-term human spaceflight and inflammaging: does it promote aging? Ageing Res Rev 87, 101909 (2023).
Garrett-Bakelman, F. E. et al. The NASA twins study: a multidimensional analysis of a year-long human spaceflight. Science (2019).
Zhou, M., Sng, N. J., LeFrois, C. E., Paul, A. L. & Ferl, R. J. Epigenomics in an extraterrestrial environment: organ-specific alteration of DNA methylation and gene expression elicited by spaceflight in Arabidopsis thaliana. BMC Genomics 20, 205 (2019).
Kojima, Y. et al. Effects of simulated microgravity on mammalian fertilization and preimplantation embryonic development in vitro. Fertil. Steril. 74, 1142–1147 (2000).
Tash, J. et al. Fertilization-critical Motility and Acrosome Reaction of Human and Bovine Sperm are Negatively Impacted by Spaceflight on the ISS (ASGSR, 2020).
Mitra, A. et al. Impact of Spaceflight Radiationand Microgravity on DNA Integrity and Fertility Risk of Human and Bovine Sperm on the ISS (ASGSR, 2020).
Matsumura, T. et al. Male mice, caged in the International Space Station for 35 days, sire healthy offspring. Sci. Rep. 9, 13733 (2019).
Mahase, E. Three FDA advisory panel members resign over approval of Alzheimer’s drug. BMJ 373, n1503 (2021).
Wakayama, S. et al. Detrimental effects of microgravity on mouse preimplantation development in vitro. PLoS ONE 4, e6753 (2009).
Yoshida, K. et al. Intergenerational effect of short-term spaceflight in mice. iScience 24, 102773 (2021).
Wakayama, S. et al. Evaluating the long-term effect of space radiation on the reproductive normality of mammalian sperm preserved on the International Space Station. Sci. Adv. (2021).
Lei, X. et al. Development of mouse preimplantation embryos in space. Natl. Sci. Rev. 7, 1437–1446 (2020).
Ho, CNQ. et al. Simulated microgravity inhibits the proliferation of chang liver cells by attenuation of the major cell cycle regulators and cytoskeletal proteins. Int. J. Mol. Sci. (2021).
Kamal, K. Y., Herranz, R., van Loon, J. J. W. A. & Medina, F. J. Simulated microgravity, Mars gravity, and 2g hypergravity affect cell cycle regulation, ribosome biogenesis, and epigenetics in Arabidopsis cell cultures. Sci. Rep. 8, 6424 (2018).
Wang, Y. et al. A major effect of simulated microgravity on several stages of preimplantation mouse development is lethality associated with elevated phosphorylated SAPK/JNK. Reprod. Sci. 16, 947–959 (2009).
Feng, M. et al. Differential expression profiles of long non‑coding RNAs during the mouse pronuclear stage under normal gravity and simulated microgravity. Mol. Med. Rep. 19, 155–164 (2019).
Li, F., Ye, Y., Lei, X. & Zhang, W. Effects of microgravity on early embryonic development and embryonic stem cell differentiation: phenotypic characterization and potential mechanisms. Front. Cell Dev. Biol 9, 797167 (2021).
Wakayama, S. et al. Development of a new device for manipulating frozen mouse 2-cell embryos on the International Space Station. PLoS ONE 17, e0270781 (2022).
Schatz, F., Guzeloglu-Kayisli, O., Arlier, S., Kayisli, U. A. & Lockwood, C. J. The role of decidual cells in uterine hemostasis, menstruation, inflammation, adverse pregnancy outcomes and abnormal uterine bleeding. Hum. Reprod. Update 22, 497–515 (2016).
Crucian, B. E. et al. Immune system dysregulation during spaceflight: potential countermeasures for deep space exploration missions. Front. Immunol. 9, 1437 (2018).
Kim, J. K. et al. Single-cell multi-ome and immune profiles of the Inspiration4 crew reveal cell-type, sex, and microbiome-specific responses to spaceflight. Nat. Commun. https://doi.org/10.1038/s41467-024-49211-2 (2024).
Abuwala, N. & Tal, R. Endometrial stem cells: origin, biological function, and therapeutic applications for reproductive disorders. Curr. Opin. Obstet. Gynecol. 33, 232–240 (2021).
Cho, H. J. et al. Microgravity inhibits decidualization via decreasing Akt activity and FOXO3a expression in human endometrial stromal cells. Sci. Rep. 9, 12094 (2019).
McMaster, M. T., Teng, C. T., Dey, S. K. & Andrews, G. K. Lactoferrin in the mouse uterus: analyses of the preimplantation period and regulation by ovarian steroids. Mol. Endocrinol. 6, 101–111 (1992).
Hennes, A. et al. Functional expression of the mechanosensitive PIEZO1 channel in primary endometrial epithelial cells and endometrial organoids. Sci. Rep. 9, 1779 (2019).
Arishe, O. O., Ebeigbe, A. B. & Webb, R. C. Mechanotransduction and uterine blood flow in preeclampsia: the role of mechanosensing piezo 1 ion channels. Am. J. Hypertens. 33, 1–9 (2020).
Proshchina, A. et al. Reproduction and the early development of vertebrates in space: problems, results, opportunities. Life (2021).
Serova, L. V. & Denisova, L. A. The effect of weightlessness on the reproductive function of mammals. Physiologist 25, S9–S12 (1982).
Serova L, D. L., Makeev, V. & Chelnaya, N. The effect of microgravity on prenatal development of mammals. Physiologist. 27, 107–110 (1984).
Ronca, A. E. & Alberts, J. R. Physiology of a microgravity environment selected contribution: effects of spaceflight during pregnancy on labor and birth at 1 G. J. Appl. Physiol. 89, 849–854 (2000). discussion 848.
Bhat, G. K., Yang, H. & Sridaran, R. Simulated conditions of microgravity suppress progesterone production by luteal cells of the pregnant rat. J. Gravit. Physiol. 8, 57–66 (2001).
Ijiri, K. Development of space-fertilized eggs and formation of primordial germ cells in the embryos of Medaka fish. Adv. Space Res. 21, 1155–1158 (1998).
Nadeem, L., Shynlova, O., Mesiano, S. & Lye, S. Progesterone via its type-A receptor promotes myometrial gap junction coupling. Sci. Rep. 7, 13357 (2017).
Lye, S. J., Nicholson, B. J., Mascarenhas, M., MacKenzie, L. & Petrocelli, T. Increased expression of connexin-43 in the rat myometrium during labor is associated with an increase in the plasma estrogen:progesterone ratio. Endocrinology 132, 2380–2386 (1993).
Kamal, D. A. M., Ibrahim, S. F. & Mokhtar, M. H. Effects of testosterone on the expression of connexin 26 and connexin 43 in the uterus of rats during early pregnancy. In Vivo 34, 1863–1870 (2020).
Burden, H. W., Zary, J. & Alberts, J. R. Effects of space flight on the immunohistochemical demonstration of connexin 26 and connexin 43 in the postpartum uterus of rats. J. Reprod. Fertil. 116, 229–234 (1999).
Keil, L., Evans, J., Grindeland, R. & Krasnov, I. Pituitary oxytocin and vasopressin content of rats flown on COSMOS 2044. J. Appl. Physiol. 73, 166S–168S (1992).
García-Ovejero, D., Trejo, J. L., Ciriza, I., Walton, K. D. & García-Segura, L. M. Space flight affects magnocellular supraoptic neurons of young prepuberal rats: transient and permanent effects. Brain Res. Dev. Brain Res. 130, 191–205 (2001).
Baer, L. A., Wade, C. E. & Ronca, A. E. Effects of hypergravity exposure on plasma oxytocin concentration in pregnant and lactating rat dams. J. Gravit. Physiol. 9, P205–P206 (2002).
Colaianni, G. et al. Bone marrow oxytocin mediates the anabolic action of estrogen on the skeleton. J. Biol. Chem. 287, 29159–29167 (2012).
Ross, A. P. et al. Sex-dependent effects of social isolation on the regulation of arginine-vasopressin (AVP) V1a, oxytocin (OT) and serotonin (5HT) 1a receptor binding and aggression. Horm. Behav. 116, 104578 (2019).
Lintault, L. M. et al. In a hypergravity environment neonatal survival is adversely affected by alterations in dam tissue metabolism rather than reduced food intake. J. Appl. Physiol. 102, 2186–2193 (2007).
Perez, M. F. & Lehner, B. Intergenerational and transgenerational epigenetic inheritance in animals. Nat. Cell Biol. 21, 143–151 (2019).
Pembrey, M. E. et al. Sex-specific, male-line transgenerational responses in humans. Eur. J. Hum. Genet. 14, 159–166 (2006).
Hardikar, A. A. et al. Multigenerational undernutrition increases susceptibility to obesity and diabetes that is not reversed after dietary recuperation. Cell Metab. 22, 312–319 (2015).
ACOG Committee Opinion No. 762: Prepregnancy counseling. American College of Obstetricians and Gynecologists. Obstet. Gynecol. 133, e78–e89 (2019).
Kominiarek, M. A. & Rajan, P. Nutrition recommendations in pregnancy and lactation. Med. Clin. North Am. 100, 1199–1215 (2016).
Jain, V. & Wotring, V. E. Medically induced amenorrhea in female astronauts. NPJ Microgravity 2, 16008 (2016).
Trussell, J. Contraceptive failure in the United States. Contraception 83, 397–404 (2011).
Heer, M. & Paloski, W. H. Space motion sickness: incidence, etiology, and countermeasures. Auton. Neurosci. 129, 77–79 (2006).
Jang, Y. S., Lee, E. S. & Kim, Y. K. Venous thromboembolism associated with combined oral contraceptive use: a single-institution experience. Obstet. Gynecol. Sci. 64, 337–344 (2021).
Marshall-Goebel, K. et al. Assessment of jugular venous blood flow stasis and thrombosis during spaceflight. JAMA Netw. Open 2, e1915011 (2019).
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Gynecology. ACOG practice bulletin no. 208: benefits and risks of sterilization. Obstet. Gynecol. 133, e194–e207 (2019).
Hibaoui, Y. & Feki, A. Organoid models of human endometrial development and disease. Front. Cell Dev. Biol. 8, 84 (2020).
Laronda, M. M. et al. A bioprosthetic ovary created using 3D printed microporous scaffolds restores ovarian function in sterilized mice. Nat. Commun. 8, 15261 (2017).
Xiao, S. et al. A microfluidic culture model of the human reproductive tract and 28-day menstrual cycle. Nat. Commun. 8, 14584 (2017).
Pantalone, D. et al. Robot-assisted surgery in space: pros and cons. A review from the surgeon’s point of view. NPJ Microgravity 7, 56 (2021).
Hiranaka, T. et al. The use of smart glasses for surgical video streaming. Surg. Innov. 24, 151–154 (2017).
El Rassi, I. & El Rassi, J. M. A review of haptic feedback in tele-operated robotic surgery. J. Med. Eng. Technol. 44, 247–254 (2020).
Sitti, M. Miniature soft robots—road to the clinic. Nat. Rev. Mater. 3, 74–75 (2018).
Zhang, Y. et al. NASA’s ground-based microgravity simulation facility. Methods Mol. Biol. 2368, 281–299 (2022).
Sarabi, M. R., Yetisen, A. K. & Tasoglu, S. Magnetic levitation for space exploration. Trends Biotechnol. 40, 915–917 (2022).
Tasoglu, S. et al. Levitational image cytometry with temporal resolution. Adv. Mater. 27, 3901–3908 (2015).
Nangle, S. N. et al. The case for biotech on Mars. Nat. Biotechnol. 38, 401–407 (2020).
Jones, J., Karouia, F., Pinsky, L. & Cristea, O. Radiation and Radiation Disorders. In Principles of Clinical Medicine for Space Flight (eds Barratt, M. R., Baker, E. S. & Pool, S. L.) 39–108 (Springer, 2019).
Patel, S. J., Reede, D. L., Katz, D. S., Subramaniam, R. & Amorosa, J. K. Imaging the pregnant patient for nonobstetric conditions: algorithms and radiation dose considerations. Radiographics 27, 1705–1722 (2007).
Megory, E. & Oyama, J. Hypergravity induced prolactin surge in female rats. Aviat. Space Environ. Med. 56, 415–418 (1985).
Tou, J. C., Grindeland, R. E. & Wade, C. E. Effects of diet and exposure to hindlimb suspension on estrous cycling in Sprague-Dawley rats. Am. J. Physiol. Endocrinol. Metab. 286, E425–433, (2004).
Forsman, A. & Nier, A. The effects of spaceflight on mucin production in the mouse uterus. Gravit. Space Res. 1, 20–28 (2013).
Schenker, E. & Forkheim, K. Mammalian mice embryo early development in weightlessness environment on STS 80 space flight. Israel Aerospace Med Inst Rep 1998, 5 (1998).
Ma, B. et al. Real-time micrography of mouse preimplantation embryos in an orbit module on SJ-8 satellite. Microgravity Sci. Technol. 20, 127–136 (2008).
Wang, Y., An, L., Jiang, Y. & Hang, H. Effects of simulated microgravity on embryonic stem cells. PLoS ONE 6, e29214 (2011).
Acharya, A. et al. Modulation of differentiation processes in murine embryonic stem cells exposed to parabolic flight-induced acute hypergravity and microgravity. Stem Cells Dev. 27, 838–847 (2018).
Lei, X. et al. Effect of microgravity on proliferation and differentiation of embryonic stem cells in an automated culturing system during the TZ-1 space mission. Cell Prolif. 51, e12466 (2018).
Oyama, J. & Platt, W. T. Reproduction and growth of mice and rats under conditions of simulated increased gravity. Am. J. Physiol. 212, 164–166 (1967).
Serova LV, D. L., Makeeva, V. F., Chelnaya, N. A. & Pustynnikova, A. M. The effect of microgravity on the prenatal development of mammals. Physiologist 27, 107–110 (1984).
Megory, E. & Oyama, J. Hypergravity effects on litter size, nursing activity, prolactin, TSH, T3, and T4 in the rat. Aviat. Space Environ. Med. 55, 1129–1135 (1984).
Moore, J. & Duke, J. Effect of chronic centrifugation on mouse breeding pairs and their offspring. Physiologist 31, S120–S121 (1988).
Burden, H. W. et al. Effects of space flight on ovarian-hypophyseal function in postpartum rats. J Reprod. Fertil. 109, 193–197 (1997).
Wong, A. M. & DeSantis, M. Rat gestation during space flight: outcomes for dams and their offspring born after return to Earth. Integr. Physiol. Behav. Sci. 32, 322–342 (1997).
Burden, H. W., Poole, M. C., Zary, J., Jeansonne, B. & Alberts, J. R. The effects of space flight during gestation on rat uterine smooth muscle. J. Gravit. Physiol. 5, 23–29 (1998).
Yang, H., Bhat, G. K. & Sridaran, R. Clinostat rotation induces apoptosis in luteal cells of the pregnant rat. Biol. Reprod. 66, 770–777 (2002).
Casey, T., Patel, O. V. & Plaut, K. Transcriptomes reveal alterations in gravity impact circadian clocks and activate mechanotransduction pathways with adaptation through epigenetic change. Physiol. Genomics 47, 113–128 (2015).
Steller, J. G., Ronca, A., Powell, T. L. & Jansson, T. Effects of near-continuous low-dose neutron irradiation on pregnancy outcomes in mice. Am. J. Obstetr. Gynecol. 222, S570–S571 (2019).